- Review
- Open access
- Published:
Advancing environmental health sciences through implementation science
Environmental Health volume 21, Article number: 136 (2022)
Abstract
Background
Environmental health sciences have identified and characterized a range of environmental exposures and their associated risk for disease, as well as informed the development of interventions, including recommendations, guidelines, and policies for mitigating exposure. However, these interventions only serve to mitigate exposures and prevent disease if they are effectively disseminated, adopted, implemented, and sustained.
Main body
Numerous studies have documented the enormous time lag between research and practice, noting that dissemination and implementation are not passive processes but rely on active and intentional strategies. Implementation science seeks to build the knowledge base for understanding strategies to effectively disseminate and implement evidence and evidence-based interventions, and thus, bridge the research-to-practice gap.
Conclusion
Environmental health researchers are well positioned to advance health promotion and disease prevention by incorporating implementation science into their work. This article describes the rationale for and key components of implementation science and articulates opportunities to build upon existing efforts to advance environmental health supported by the National Institute of Environmental Health Sciences and National Institutes of Health broadly.
Background
The National Institute of Environmental Health Sciences (NIEHS) seeks to understand “how the environment affects people in order to promote healthier lives.” NIEHS has invested substantially in environmental health research which has enumerated scores of chemicals that may cause disease, elucidated molecular mechanisms for disease initiation and progression, and informed the development of interventions, including recommendations, guidelines, and policies for mitigating exposure. However, these evidence-based interventions, recommendations, guidelines, and policies (hereafter referred to collectively as “interventions”) are only effective at mitigating exposures and preventing disease if they are effectively disseminated, adopted, implemented, and sustained.
Numerous studies have documented the enormous time lag between clinical research and practice. While in healthcare this estimate has hovered around 17 years [1, 2], the time lag can be substantially longer for environmental health evidence to result in changes to policy and practice. For example, we continue to see high rates of smoking despite the 1964 Surgeon General Report and effective tobacco control interventions including those which reduce exposure to secondhand smoke in the workplace. Air pollution is another example. Despite significant documentation of mortality associated with air pollution as early as the 1950s [3], the Clean Air Act wasn’t established until 1970 and air pollution continues to plague many U.S. cities. Even longer lags have been seen with arsenic, which we’ve known is carcinogenic for over a century, yet arsenic levels in the U.S. population continue to be above the U.S. Federal Government’s national health objectives goal as outlined in Healthy People 2020. Other examples include lead and mercury, for which it took decades for the evidence on their health effects to translate to global policy action [4], and yet millions of children continue to be exposed to high levels of these toxins.
Increasingly researchers have come to appreciate that dissemination and implementation of evidence-based interventions are not passive processes but rely on active and intentional strategies that should be informed by theories, stakeholders, and evidence. Implementation science seeks to build the knowledge base for understanding strategies to effectively disseminate, implement, and sustain evidence and evidence-based interventions, and thus, bridge the research-to-practice gap [5, 6]. Given the complex influences and global nature of environmental exposures, environmental health researchers are well positioned to advance disease prevention by integrating implementation science into their work.
In this article, we describe the key components of implementation science and articulate ways that environmental health researchers can build upon existing efforts to advance environmental health through implementation science. NIEHS emphasizes the importance of engaging with affected communities, practitioners, policymakers, and other partners across multiple sectors, and the need to develop and equitably implement effective, evidence-based environmental health interventions to prevent and mitigate harmful exposures and reduce environmental health disparities. Table 1 provides a roadmap for environmental health scientists to consider how implementation science could advance their work in alignment with NIEHS goals. Further, we provide an example of a network of environmental health researchers and implementation scientists collaborating to advance the implementation of clean cookstove interventions to reduce household air pollution and improve population health. We hope this example may serve to drive future research directions and collaborations.
What is implementation science?
Implementation science is the study of methods to promote the adoption and integration of evidence and evidence-based practices, interventions and policies into routine healthcare and community settings to improve health [5, 6]. The National Institutes of Health (NIH) issued funding announcements in 2005 to support research on understanding barriers to dissemination and implementation and develop and test strategies to overcome those barriers.
For the purposes of the funding announcements, the NIH makes a distinction between dissemination research and implementation research. Dissemination research is defined as the study of the “targeted distribution of information and intervention materials to a specific public health, clinical practice, or policy audience” [5]. The intent is to understand how, when, by whom, and under what circumstances evidence and the associated evidence-based interventions can be most effectively communicated and integrated into practice. It accounts for all the stages of dissemination, including the creation, packaging, transmission, and reception of the knowledge and associated interventions. These are steps we often take for granted but that can impact the effectiveness of our dissemination efforts.
Implementation research has been defined as the study of the use of strategies to adopt and integrate evidence-based health interventions into clinical and community settings to improve individual outcomes and benefit population health [5]. While clinical trials test the effectiveness of interventions to improve health outcomes, implementation research focuses on understanding how those interventions can best be delivered to ensure they have the intended impact on health. Implementation studies develop and test strategies to ensure effective implementation. Rather than focusing on individual health outcomes, implementation studies focus on proximal outcome measures that demonstrate implementation success, such as measures of acceptability, adoption, appropriateness, costs, feasibility, fidelity, penetration, and sustainability [12]. The goal is to identify a strategy or set of strategies that will maximize effective adoption, implementation and sustainability of an evidence-based intervention, and thus, ultimately improve population health. Additional key components of implementation science are described in the following paragraphs with a guiding example from environmental health on the adoption and use of clean cookstoves to reduce household air pollution. This example comes from the Clean Cooking Implementation Science Network, which was established and funded by the National Institutes of Health in partnership with the Environmental Protection Agency (EPA), Centers for Disease Control and Prevention (CDC), U.S. Agency for International Development (USAID), and the Clean Cooking Alliance. The network consists of environmental health researchers and implementation scientists studying strategies to promote the adoption, use, and scale-up of clean cooking technologies around the globe.
Theories, frameworks, and models
The field of implementation science hinges on theories, frameworks, and models to inform dissemination and implementation processes and help determine the most effective strategies to overcome barriers to dissemination and implementation. These theories, frameworks, and models (hereafter referred to collectively as frameworks) typically recognize the importance of context as well as the multiple levels of influence on dissemination and implementation processes. More than 60 frameworks are used in the field [13] for a variety of purposes including to inform processes and determinants of implementation, as well as to evaluate implementation success [14].
Some of the most commonly used frameworks in NIH-funded studies include Everett Rogers’ Diffusion of Innovations [15] and the Consolidated Framework for Implementation Research [16], both of which posit that the decision to adopt and successfully implement an intervention is influenced not only by the characteristics of the intervention itself but also by the setting or context in which that intervention is implemented. Further, these frameworks recognize the multiple levels of influence in a given context, from the organizational or community setting to the broader municipality, state, or nation. For example, the decision to adopt and implement a clean cookstove, such as a liquid purified gas (LPG) stove, in a household will be influenced not only by whether that cookstove is relatively simple to use, but also whether the household member(s) can access the gas required to power the stove or have access to technical assistance to use or repair the stove. The decision will also be based on cultural and behavioral factors in the home and community, which often drive adoption and acceptance. These frameworks guide our studies by informing our hypotheses about how interventions work, why they work, and what might impede or support the ability to implement them, which can inform a priori strategies to facilitate implementation.
The selection of frameworks will depend on the research questions and study objectives. In the clean cookstoves example, researchers used the RE-AIM Framework to understand the Reach, Effectiveness, Adoption, Implementation, and Maintenance of clean cookstoves across 11 low- and middle-income countries. This enabled them to identify key gaps in implementation and highlight areas for future efforts.
One important feature of implementation science frameworks is their attentiveness to multi-level factors that influence implementation, including characteristics of 1) the individuals delivering the intervention, 2) the organization in which it is delivered, and 3) the community in which those individuals and organization exist. This is critical for environmental health studies that seek to eliminate health disparities. Understanding contextual factors that influence equitable implementation can help us design and deliver interventions that will mitigate and not exacerbate existing environmental health disparities disproportionately affecting communities of color.
Implementation strategies
Implementation strategies are the focus of implementation science. They are defined as the “methods or techniques used to enhance the adoption, implementation and sustainability of an evidence-based program or practice” [17]. Most implementation studies seek to develop and test strategies to improve uptake and use of effective interventions. The purpose of these strategies is to improve the aforementioned proximal outcomes, such as the feasibility, adoption, or sustainability of an intervention [12]. Over 70 strategies have been classified into broad categories [17, 18], including evaluative and iterative strategies, interactive assistance, adapting and tailoring to context, developing stakeholder relationships, educating and training, engaging consumers, financial strategies, and strategies to change infrastructure. The selection of a strategy or set of strategies will depend on the implementation barriers being addressed and the implementers being targeted. For example, in efforts to overcome financial barriers for households to use LPG stoves, investigators tested conditional cash transfers as a financial incentive for adoption and use. In seeking to influence policymakers at the municipal, state, or national level for LPG stove distribution, studies might test strategies to develop stakeholder relationships and build buy in. Examples of these types of strategies include identifying champions, informing local opinion leaders, or building coalitions. If a major barrier is the ability to properly use and maintain the stove, studies might focus on strategies to provide interactive assistance, such as facilitation or technical assistance. Ultimately, implementation science seeks to understand which set of strategies work best in a particular context to improve implementation outcomes.
Study designs
Implementation science uses a variety of study designs typically used in other fields, including observational and experimental designs. Study designs that may be less familiar to environmental health researchers but that are commonly used in implementation science include quasi-experimental and effectiveness-implementation hybrid designs, as well as mixed methods designs [19]. The following paragraphs will review some of these designs in more detail and provide guiding examples.
Experimental designs
One popular experimental design is the stepped wedge design [20], which is a type of cluster randomized controlled trial (RCT). In the stepped wedge design an intervention is rolled out in multiple places (or clusters) sequentially rather than simultaneously, and comparisons can be made within and between clusters. The advantage of this design is that it is more feasible to focus resources in one place at a time. This can be particularly useful for a clean cookstove intervention trial that seeks to test strategies across multiple community settings but may not have the resources to implement the intervention across all settings at one time.
Quasi-experimental designs
While experimental designs test an intervention through randomization, quasi-experimental designs were developed to test interventions when randomization is not possible. This is often the case when pursuing questions related to mitigation or reduction of exposures to environmental pollutants. These include designs such as interrupted time series [21], regression discontinuity [22], and non-equivalent control group [23]. These designs are particularly useful in environmental health where it may be unethical to withhold an intervention that can prevent or reduce exposure harms. For example, in an interrupted time series (ITS) design everyone receives the intervention and multiple assessments are taken prior to and following the introduction of the intervention. An ITS design could be an appropriate design to study the impact and rollout of a lead abatement program which would be implemented broadly, including all eligible households in a community rather than withholding abatement from some participants. In selecting a study design, careful attention should be paid to the underlying assumptions, advantages, and disadvantages.
Hybrid designs
Effectiveness-implementation hybrid designs are another particularly useful design for environmental health researchers developing interventions. These designs have a dual focus a priori on assessing intervention effectiveness and implementation [24]. The overall goal is to accelerate the transition from effectiveness studies to implementation studies. There are three types of hybrid designs that vary by the emphasis placed on the aims of the study. At one end of the spectrum, Type 1 designs are primarily focused on studying intervention effectiveness while secondarily collecting information about implementation processes including barriers to implementation. For example, in developing an early warning system for disaster preparedness, researchers can test the effectiveness of the system in its ability to predict and monitor conditions allowing for communities to prepare for and adapt to disasters, while also studying how such a system would be implemented in a particular context (e.g., how would data be accessed, how would the system be run and maintained, how would output reach the affected communities, who would be ensuring these steps take place, etc.) At the other end of the spectrum, Type 3 designs are primarily focused on testing implementation strategies while secondarily collecting information on health outcomes. For example, researchers developed and tested an effective household intervention that increased the appropriate and exclusive use of clean cooking technologies through education, incentivization, and environmental restructuring [25, 26]. In a subsequent type 3 hybrid design, researchers could develop and test strategies that will support the ability to scale up the intervention across a range of settings while also assessing the intervention’s effectiveness to increase use of clean cookstoves, for example, through air monitoring to measure reductions in indoor air pollution. Type 2 designs fall in between Type 1 and Type 3 designs, with a dual primary focus of testing effectiveness and testing an implementation strategy. The type of hybrid design selected is dependent on the degree to which effectiveness of an intervention is already well characterized for a particular context. These designs offer an opportunity for environmental health researchers who are focusing on prevention to not only test the effectiveness of their interventions but also understand implementation processes required to deliver the intervention in a variety of settings. Understanding these processes and identifying the appropriate people to implement an intervention are the first steps in understanding factors that influence successful implementation, enabling subsequent implementation studies on strategies to increase the likelihood that these interventions will be effectively delivered in practice.
Mixed methods
Mixed methods designs are the collection and integration of qualitative and quantitative data to help understand processes and context. Where quantitative data can provide a measure of effect, qualitative data can reveal the reasons why and how things work or don’t work. For example, in a clean cookstove study that tests strategies to enhance LPG stove adoption and use, investigators may measure uptake and use by measuring particulate matter levels in household ambient air and may also use direct observation and/or conduct qualitative interviews and focus groups to understand how and why households used or did not use the LPG stoves. Understanding why a strategy to enhance implementation was effective or not allows for an iterative process to modify or adapt an intervention to fit a specific context, or to further refine a set of strategies to enhance implementation.
For environmental health researchers who have historically focused on documenting risks and understanding their causes, implementation science can further expedite efforts that shift the scientific focus towards better understanding how to promote prevention. Through focusing on the how, we can advance disease prevention and improve population health by understanding the most effective strategies that enable us to effectively communicate, integrate, and sustain interventions (including recommendations, guidelines, and policies) in practice. The following section enumerates ways that environmental health researchers can incorporate implementation science into their work at various stages of the translational research pathway, to bridge the gap from research to practice.
Integrating implementation science into environmental health sciences
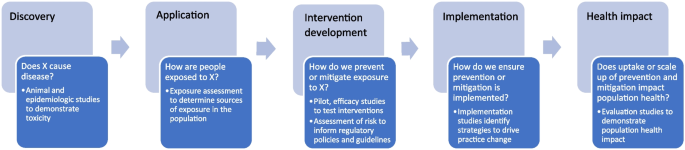
Many have articulated the translational research pathway from basic discovery to human application to intervention development to implementation and evaluation [27,28,29]. However, these earlier models were developed primarily for medical research. More recently, the NIEHS developed the Translational Research Framework (https://www.niehs.nih.gov/research/programs/translational/framework-details/index.cfm) which serves as a guide for environmental health scientists to envision how their studies can move along this pathway. Importantly, this framework highlights the development of evidence-based interventions and implementation science playing key roles in this iterative (and not always linear) process [30]. Figure 1 illustrates the translational research pathway in the context of environmental health research, elaborating on the role of implementation science.
Much of environmental health research has focused on the first stages of this pathway, from basic discovery to application to intervention development, namely, informing recommendations, guidelines, and regulatory policies, as well as health interventions. For example, environmental health researchers have made substantial progress in basic discovery by identifying and characterizing chemical toxicity through in vitro, in silico, animal, and epidemiologic studies. These discoveries have led to research that focuses on the underlying mechanisms by which these exposures impact biology and pathophysiology and research on understanding how people are exposed to these chemicals across the lifespan in multiple environments. Through exposure assessments, environmental health researchers have elucidated the relevant chemical species and main sources of exposure. This application then leads to science that would inform the development of policies, recommendation, and guidelines, such as risk assessments that would reduce exposures to a safe level in a population. Further, understanding the relevant sources of exposure can inform prevention or mitigation efforts. Thus, interventions can be developed that can prevent or mitigate human exposure to these relevant sources. For example, to reduce exposure to household air pollution, a variety of clean cooking technologies have been developed for households with unreliable access to electricity or gas. However, these clean cookstove technologies are not necessarily being adopted nor used appropriately by households [31]. Once interventions are developed and tested, implementation studies can inform the most effective strategies to ensure their adoption and appropriate use, and ultimately, how best to scale up these interventions to all populations who can benefit. In the example of cookstoves, the Clean Cooking Implementation Science Network [31] has studied a range of strategies to promote adoption and appropriate use, including strategies to increase awareness [32] and financial strategies to incentivize replacement of polluting stoves [33]. Finally, evaluation studies can assess the health impact of these implementation and scale up efforts [34].
Implementation science has evolved and developed methods not only to focus on the later stages of the translational research pathway, but also to inform intervention development studies. In studying human application and intervention development, researchers should consider who will be delivering the intervention and how it fits with the ultimate consumer population, and build in tests of training, support, and adherence. For example, effectiveness-implementation hybrid designs, whereby researchers can dually study intervention effectiveness as well as implementation [24], as described above in the examples of early warning systems and clean cookstoves, can help to speed up the translational research process by integrating implementation studies and intervention development studies. By designing interventions for dissemination and implementation, researchers can increase the likelihood that the outputs of their research will be implemented in practice. For example, the Household Air Pollution Intervention Network Trial is a multi-country trial testing the effectiveness of clean cooking technologies on improving health outcomes [35] while also studying approaches to improve use of the clean cookstoves [36].
We have a tremendous opportunity to use implementation science to understand how environmental health evidence is being disseminated, implemented, and sustained, and how best to address the gaps in those processes. Institutes, centers, and offices across the NIH recognize the importance of advancing our understanding of the most effective strategies to integrate evidence-based interventions within community, clinical, and public health systems. Thus, they have issued a set of funding announcements in Dissemination and Implementation Research in Health (PAR-22-105, PAR-22-106, PAR-22-109), which seek to build the knowledge base on how to effectively disseminate, implement, sustain, and scale evidence-based interventions, as described in the previous section. These institutes and centers include several focused on environmental exposures, including NIEHS, National Cancer Institute (NCI), Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Mental Health, National Heart, Lung, and Blood Institute, and Fogarty International Center. At NIEHS, the integration of implementation science is developing throughout the portfolio, including a new initiative on children’s health that supports collaborations between environmental health scientists and implementation scientists (https://grants.nih.gov/grants/guide/rfa-files/rfa-es-20-001.html). NIEHS supported scientists are also involved in the NIH-wide RADxUP program which is conducting implementation science related to the uptake of COVID19 testing in communities experiencing health disparities and environmental injustice.
In addition to funding opportunities, NIH supports a range of training opportunities. For example, the NCI hosts the Training Institute in Dissemination and Implementation Research in Cancer (TIDIRC), which provides thorough instruction in conducting dissemination and implementation studies and is now available in open access format (https://cancercontrol.cancer.gov/IS/training-education/tidirc/openaccess.html). Additional implementation science resources for environmental health researchers can be found at the NIEHS website (https://www.niehs.nih.gov/research/supported/translational/implementation/index.cfm) and the NCI Implementation Science Team website (https://cancercontrol.cancer.gov/IS/).
Conclusions
Environmental health researchers can advance disease prevention not only by informing the development of effective interventions, regulatory policies, and guidelines, but also by ensuring that those interventions, policies, and guidelines are effectively adopted, implemented and sustained. They can do this by incorporating implementation science into their work across the translational research pathway. Namely, environmental health researchers can design interventions that better fit the context in which they are meant to be applied. Further, they can study implementation processes and inform implementation strategies to most effectively implement those interventions. A variety of methods and study designs in implementation science have been described in this paper that can guide environmental health researchers to conduct implementation studies. By fully integrating the concepts, methods, and findings of implementation science into the environmental health research agenda, we can envision a more comprehensive flow from research to practice that maximizes the use of scientific discovery and supports the NIEHS mission of discovering how the environment affects people in order to promote healthier lives.
References
Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform. 2000;1:65–70.
Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510–20.
Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360(9341):1233–42.
UN. Global sustainable development report: United Nations; 2015.
NIH. Dissemination and Implementation Research in Health Program Announcement (R01 Clinical Trial Optional) 2022 [Available from: https://grants.nih.gov/grants/guide/pa-files/PAR-22-105.html.]
Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci. 2006;1(1):1.
Brownson RC, Kumanyika SK, Kreuter MW, Haire-Joshu D. Implementation science should give higher priority to health equity. Implement Sci. 2021;16(1):28.
Kumar P, Dover RE, Díaz-Valdés Iriarte A, Rao S, Garakani R, Hadingham S, et al. Affordability, accessibility, and awareness in the adoption of liquefied petroleum gas: a case-control study in rural India. Sustainability. 2020;12(11):4790.
Ronzi S, Puzzolo E, Hyseni L, Higgerson J, Stanistreet D, Hugo MNB, et al. Using photovoice methods as a community-based participatory research tool to advance uptake of clean cooking and improve health: the LPG adoption in Cameroon evaluation studies. Soc Sci Med. 2019;228:30–40.
Johnson K, Gustafson D, Ewigman B, Provost L, Roper R. Using rapid-cycle research to reach goals: awareness, assessment, adaptation, acceleration in: quality AfHRa, editor. Bethesda, MD. 2015;2015.
Metz A, Woo B, Loper A. Equitable implementation at work. Stanf Soc Innov Rev. 2021;19(3):A29–31.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Admin Pol Ment Health. 2011;38(2):65–76.
Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43(3):337–50.
Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53.
Rogers EM. Diffusion of innovations, vol. xxi. 5th ed. New York: Free Press; 2003. p. 551.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. 2015;10:21.
Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the expert recommendations for implementing change (ERIC) study. Implement Sci. 2015;10:109.
Brown CH, Curran G, Palinkas LA, Aarons GA, Wells KB, Jones L, et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. 2017;38:1–22.
Hemming K, Haines TP, Chilton PJ, Girling AJ, Lilford RJ. The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ. 2015;350:h391.
Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750.
Venkataramani AS, Bor J, Jena AB. Regression discontinuity designs in healthcare research. BMJ. 2016;352:i1216.
Krishnan P. A review of the non-equivalent control group post-test-only design. Nurse Res. 2019;26(2):37–40.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–26.
Thompson LM, Diaz-Artiga A, Weinstein JR, Handley MA. Designing a behavioral intervention using the COM-B model and the theoretical domains framework to promote gas stove use in rural Guatemala: a formative research study. BMC Public Health. 2018;18(1):253.
Williams KN, Thompson LM, Sakas Z, Hengstermann M, Quinn A, Díaz-Artiga A, et al. Designing a comprehensive behaviour change intervention to promote and monitor exclusive use of liquefied petroleum gas stoves for the Household Air Pollution Intervention Network (HAPIN) trial. BMJ Open. 2020;10(9):e037761.
Zerhouni EA. Clinical research at a crossroads: the NIH roadmap. J Investig Med. 2006;54(4):171–3.
Khoury MJ, Gwinn M, Ioannidis JP. The emergence of translational epidemiology: from scientific discovery to population health impact. Am J Epidemiol. 2010;172(5):517–24.
Fort DG, Herr TM, Shaw PL, Gutzman KE, Starren JB. Mapping the evolving definitions of translational research. J Clin Transl Sci. 2017;1(1):60–6.
Pettibone KG, Balshaw DM, Dilworth C, Drew CH, Hall JE, Heacock M, et al. Expanding the concept of translational research: making a place for environmental health sciences. Environ Health Perspect. 2018;126(7):074501.
Rosenthal J, Balakrishnan K, Bruce N, Chambers D, Graham J, Jack D, et al. Implementation science to accelerate clean cooking for public health. Environ Health Perspect. 2017;125(1):A3–a7.
Kumar P, Dhand A, Tabak RG, Brownson RC, Yadama GN. Adoption and sustained use of cleaner cooking fuels in rural India: a case control study protocol to understand household, network, and organizational drivers. Arch Public Health. 2017;75:70.
Harrell BS, Pillarisetti A, Roy S, Ghorpade M, Patil R, Dhongade A, et al. Incentivizing elimination of biomass cooking fuels with a reversible commitment and a spare LPG cylinder. Environ Sci Technol. 2020;54(23):15313–9.
Quinn AK, Bruce N, Puzzolo E, Dickinson K, Sturke R, Jack DW, et al. An analysis of efforts to scale up clean household energy for cooking around the world. Energy for Sustainable Dev. 2018;46:1–10.
Clasen T, Checkley W, Peel JL, Balakrishnan K, McCracken JP, Rosa G, et al. Design and rationale of the HAPIN study: a multicountry randomized controlled trial to assess the effect of liquefied petroleum gas stove and continuous fuel distribution. Environ Health Perspect. 2020;128(4):047008.
Hengstermann M, Díaz-Artiga A, Otzóy-Sucúc R, Laura Maria Ruiz-Aguilar A, Thompson LM, Aravindalochanan V, et al. Developing visual messages to support liquefied petroleum gas use in intervention homes in the household air pollution intervention network (HAPIN) trial in rural Guatemala. Health Educ Behav. 2021;48(5):651–69.
Acknowledgements
The authors wish to acknowledge David Chambers at the National Cancer Institute for reading the manuscript and providing feedback. Additionally, the authors thank Curt DellaValle at the National Cancer Institute for serving as a sounding board in the development of this commentary.
Funding
Open Access funding provided by the National Institutes of Health (NIH). No financial support was provided for this work.
Author information
Authors and Affiliations
Contributions
GN conceived of and led the development and writing of the manuscript. LM contributed to the writing of sections of the manuscript, including developing the table. GC provided substantial input on the manuscript and development of the table. All authors contributed to the writing of the manuscript, revising it critically for important intellectual content. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Neta, G., Martin, L. & Collman, G. Advancing environmental health sciences through implementation science. Environ Health 21, 136 (2022). https://doi.org/10.1186/s12940-022-00933-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-022-00933-0